Bubble Continuous Positive Airway Pressure (bCPAP) has arrived in Kiambu! Just why this is so exciting will probably be lost on anyone who is unfamiliar with bCPAP, so here’s a quick description of what it is.
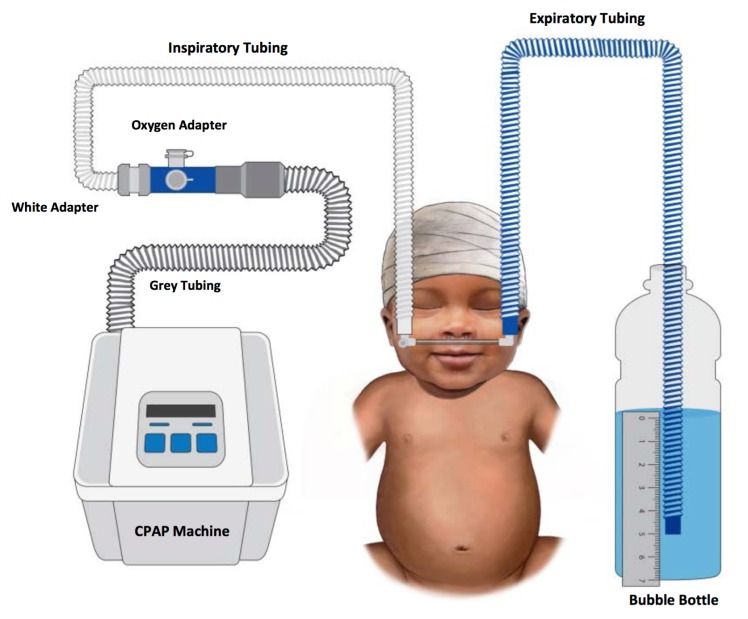
Our lungs are made up of between 300 and 500 million tiny air pockets called alveoli, across which gas is exchanged. If it were possible to lay our lungs out flat, it’s estimated that they would have a surface area the same as one half of a tennis court. Alveoli could be compared to small balloons, and like a balloon, when they collapse down completely they require a a large amount of force to start inflating them. bCPAP is a simple system to deliver a constant flow of gas (air ± additional oxygen) to a patient to keep their their alveoli from collapsing down completely and ease the effort they need to exert in order to breathe. It can mean the difference between recovering from pneumonia (and other causes of respiratory distress) and requiring intensive care. And in Kiambu, we have very limited access to intensive care for our patients.

We had 3 days of training led by the Kenyan Paediatric Association, and the team from Colombia University: Patrick Wilson and Megan Benckert. The aim of the training, was to train trainers, so that the bCPAP programme can be self sustaining. The first day consisted of the theory behind how bCPAP works, the indications for therapy, contraindications to therapy, potential complications of therapy and eventually how to set up the equipment on a patient. The following days consolidated this learning and went on to train those on the course how to train other staff. The final day concentrated on how to care for the equipment, before going to the ward, introducing the rest of the staff to bCPAP and finally putting a patient with respiratory distress on to bCPAP.
For those who are interested in some of the evidence for the effectiveness of bCPAP, it has been show to be beneficial for a variety of causes of respiratory distress in children up to the age of 5. Kawaza, et al. (2014) demonstrated a 27% absolute improvement in survival in neonates with respiratory distress syndrome. Of course, cost effectiveness is an important concern in LMICs, and bCPAP has been shown to be highly cost effective. The bCPAP drivers being used in Kiambu cost around $400 (about £275, or 40,000 KSh).
I have used CPAP in various forms fairly extensively in the UK, and having spent just a few weeks in Kiambu, I have seen several patients in whom it may have been the therapy that would have made the vital difference for them. I’m looking forward to being involved in implementing it in Kiambu, and I have no doubt it will save lives.
Hey Stuart
Excellent project to get involved with. I look forward to hearing more. Is this a good opportunity to gather some good pre- and post- bCPAP data?
LikeLiked by 1 person
That’s the plan! 🙂 Just need to work out what pre- data I can dig up. Think I might be able to use the model that the Blantyre group used which was to have a control group made up of those which meet the criteria for bCPAP but can’t go on it because there’s the machines are already in use. It would be a pragmatic rather than ideal study design.
LikeLike
I really enjoyed reading this. granny (btw Granny wrote this herself)
LikeLike